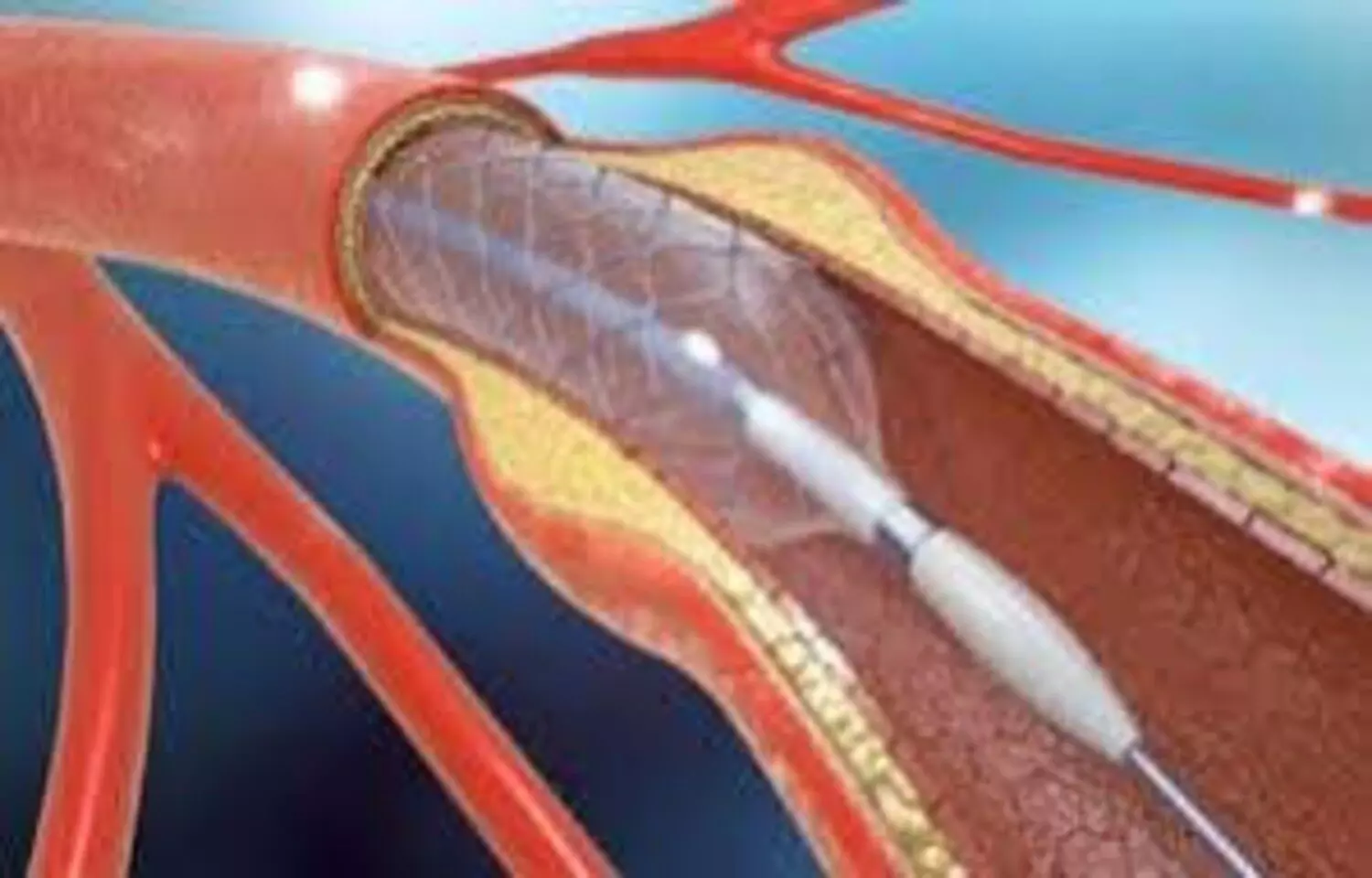
In patients with peripheral vascular disease (PVD) undergoing peripheral vascular intervention (PVI), both intravenous and oral hydration protocols were effective and safe in preventing contrast-induced nephropathy (CIN). Oral hydration was found to be non-inferior to intravenous hydration in eligible patients, offering a feasible alternative that may improve patient comfort and reduce clinical workload without compromising renal safety.Hydration therapy is recommended to prevent contrast-induced nephropathy (CIN); however, it has not been adequately studied in patients with peripheral vascular disease (PVD) undergoing peripheral vascular intervention (PVI). This study aimed to evaluate the efficacy and safety of intravenous hydration and oral hydration protocols for preventing contrast-induced nephropathy. This quasi-experimental study enrolled patients with peripheral vascular disease who were undergoing peripheral vascular intervention from September 2023 to October 2024. Patients were divided into an intravenous hydration group (receiving normal saline at a rate of 1–3 mL/kg/h for 6 h after PVI) or an oral hydration group (receiving 1000 mL of water within the first 3 h and a total of 2000 mL within 24 h after PVI). The primary endpoint was the incidence of contrast-induced nephropathy, defined as an absolute increase in serum creatinine of more than 26.5 µmol/L within 48 h. The secondary outcomes included renal function indicators (serum creatinine, blood urea nitrogen, and serum uric acid) at 48 h post-surgery; the incidence of adverse reactions (gastrointestinal adverse reactions, infusion-related adverse reactions, and electrolyte imbalances) within 24 h; and the incidence of major adverse events (acute kidney injury stage 3, acute heart failure, and all-cause mortality) during hospitalization and within 7 days after discharge.Results: A total of 560 patients with peripheral vascular disease were enrolled in the study. The overall incidence of contrast-induced nephropathy was 3.93% (22/560), with 3.60% (10/278) in the intravenous hydration group and 4.26% (12/282) in the oral hydration group, showing no statistically significant difference (p > 0.05). No statistically significant differences were observed between the two groups in the 48-hour postoperative levels of serum creatinine, blood urea nitrogen, or serum uric acid (p > 0.05). Five patients in the IV hydration group developed non-thrombotic phlebitis, and 3 patients in the oral hydration group experienced gastrointestinal adverse reactions, including nausea (n = 2) and vomiting (n = 1). None of the patients experienced electrolyte imbalances or major adverse events.For patients with peripheral vascular disease undergoing peripheral vascular intervention, both the intravenous hydration and oral hydration protocols used in this study were effective and safe in preventing contrast-induced nephropathy. These findings support the feasibility of oral hydration as a non-inferior alternative in eligible patients, potentially enhancing patient comfort and reducing clinical burden.Reference:Liu, J., Zhu, H. & Liu, L. Comparison of intravenous hydration and oral hydration in preventing contrast-induced nephropathy among patients undergoing peripheral vascular interventions. BMC Nephrol (2026). https://doi.org/10.1186/s12882-025-04737-5Keywords:Oral, Hydration, Safe, Effective, Alternative, IV Hydration, contrast-induced, nephropathy, Prevention, Study, Liu, J., Zhu, H. & Liu, L, BMC Nephrology, Peripheral vascular disease, Peripheral vascular interventions, Contrast-induced nephropathy, Intravenous hydration, Oral hydration