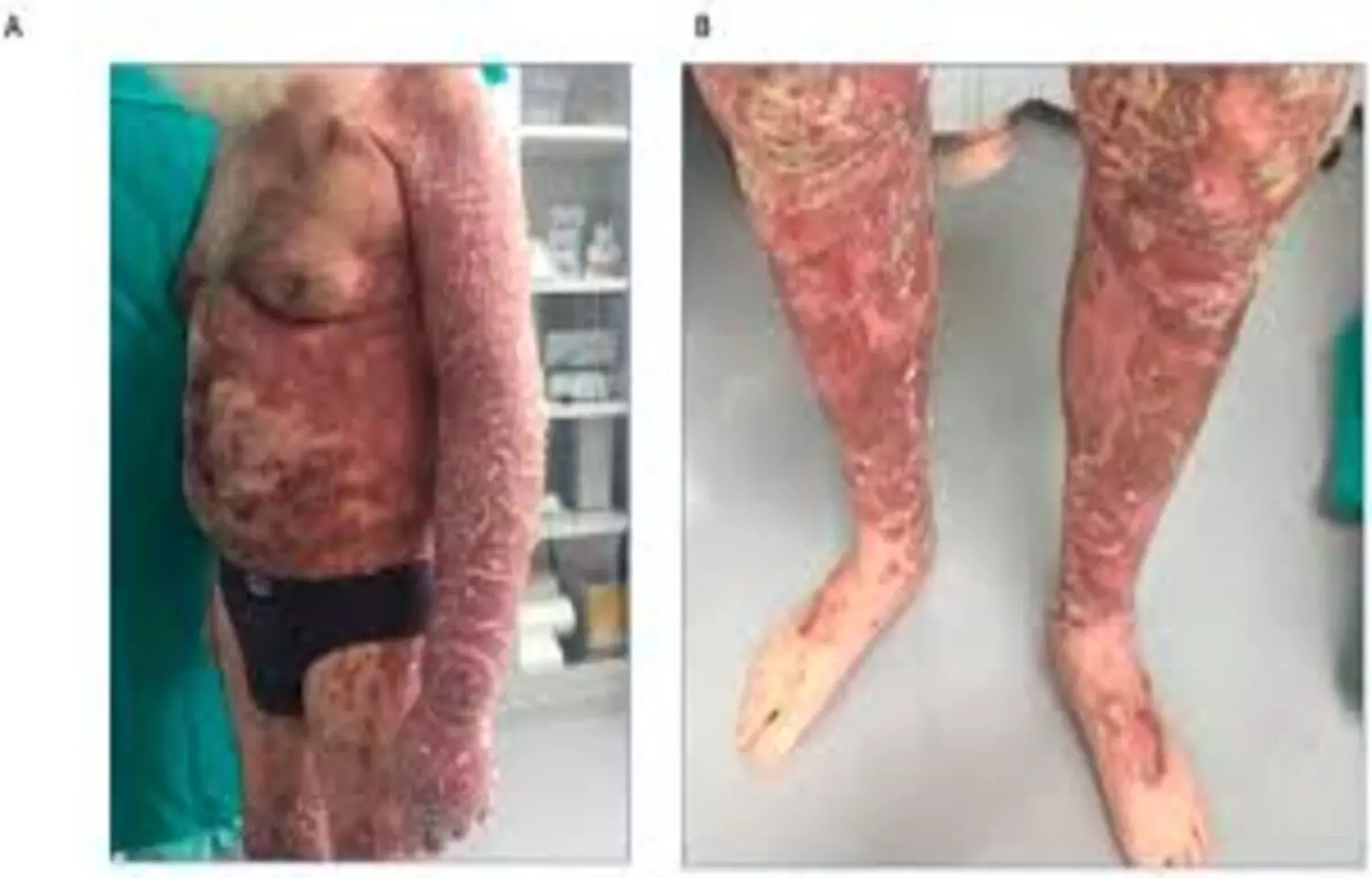
Over 52 weeks of treatment, risankizumab led to significant improvements in both clinical outcomes and optical coherence tomography (OCT) parameters, highlighting the value of long-term therapy in psoriasis. The findings show that therapeutic benefits extend beyond visible skin improvement, with optical coherence tomography serving as a useful tool to assess deeper vascular treatment responses and provide a more comprehensive evaluation of treatment efficacy.Psoriasis is a chronic inflammatory disease associated with multiple systemic comorbidities and reduced quality of life. Risankizumab, an interleukin (IL)-23 inhibitor, has demonstrated efficacy in achieving rapid and sustained skin clearance in moderate-to-severe psoriasis. However, its impact on chronic subclinical inflammation is less understood. Conventional clinical assessments like Psoriasis Area and Severity Index (PASI), Investigator’s Global Assessment (IGA), and Body Surface Area (BSA) focus on evaluating visible symptoms and are limited in capturing underlying disease activity. Optical coherence tomography (OCT), a non-invasive imaging modality, offers real-time assessment of structural and vascular changes, providing valuable insights beyond the skin surface. This sub-analysis of a prospective, single-centre exploratory study included 22 patients with moderate-to-severe psoriasis treated with risankizumab. Clinical assessments (PASI, IGA, BSA) were conducted at baseline and weeks 2, 4, 16, 28, 40, and 52. Optical coherence tomography imaging performed at baseline and weeks 4, 16, and 52 evaluated epidermal thickness and vascular parameters (e.g., vessel density and diameter) in lesional and perilesional skin.Results: By week 16, mean (95% confidence interval [CI]) PASI score decreased from 16.3 (11.6–21.1) at baseline to 3.5 (1.8–5.2), and BSA involvement from 24.7% (16.1–33.3) to 5.2% (1.9–8.4) (both p < 0.001). By week 52, 86.7%, 73.3%, and 40.0% of patients achieved PASI 75, 90, and 100, respectively, and 93.3% achieved Investigator’s Global Assessment 0/1. Optical coherence tomography showed lesional reductions in epidermal thickness (− 37.4%), vessel density (− 26.6% Δ area under the curve [AUC]), and vessel diameter (− 59.5% ΔAUC) over the 52 weeks. Notably, vascular changes also occurred in uninvolved perilesional skin.Risankizumab improved both clinical and optical coherence tomography parameters over 52 weeks, emphasising the importance of long-term therapy with benefits extending beyond visible improvement. Optical coherence tomography emerged as a valuable tool for assessing deep (vascular) treatment response, thereby supporting a more comprehensive understanding of therapeutic outcomes in psoriasis.Reference:Zirpel, H., Ha-Wissel, L., Hobelsberger, S. et al. Evaluating Risankizumab’s Long-Term Effects in Psoriasis Using Optical Coherence Tomography. Dermatol Ther (Heidelb) (2026). https://doi.org/10.1007/s13555-025-01637-2Keywords:Risankizumab, Demonstrates, Sustained, Clinical, OCT, Improvements, Psoriasis, Study, Zirpel, H., Ha-Wissel, L., Hobelsberger, S, Psoriasis, Risankizumab, Optical coherence tomography, Interleukin-23